Computer simulation could become 'integral' in the diagnosis, treatment, or prevention of disease by the end of the century
The life-saving, real-time techniques are close, but each NHS scandal is a setback for virtual medicine
A patient is rushed to hospital after suffering a severe stroke. Immediate action is needed to return blood to the affected part of their brain; without this they may suffer brain damage or die. Poised to begin surgery, doctors are warned by real-time computer simulations that show how the blood is flowing around the patient's brain that the consequences of their actions could be dire. Equipped with this information, they change course, and the patient survives.
Such a scenario, where computers are relied upon to make calculations that even the best brain surgeon could not, sounds fantastical. But this is exactly the sort of medical advance the authors of a groundbreaking new book, due to be launched tomorrow, argue is within touching distance.
Computational Biomedicine: Modelling the Human Body is the world's first textbook dedicated to the direct use of computer simulation in the diagnosis, treatment, or prevention of a disease. It claims that such technology will be "integral" to the way clinical decisions are made in the UK's operating theatres by the end of this century.
Arguing that medicine is "on the verge of a radical transformation driven by the inexorably increasing power of information technology", it predicts that drugs will soon be selected on the basis of an individual patient's "digital profile", so treatments can be tailor-made to suit them.
One of the book's authors is Professor Peter Coveney, director of the University College London Centre for Computational Science. He argues that the very fact of its publication proves the discipline has moved beyond theory and should be embraced by doctors, some of whom remain sceptical. "There's something very significant that's going on," he said. "It's no longer just a research activity, it's getting to the stage where one can write a textbook and say 'this is the way things work in this field' without being overly detailed and niche."
Recent advances in computer-simulated medicine were discussed last month at a conference at the University of Sheffield, where the Insigneo Institute was founded a year ago. It comprises 123 academics and clinicians working towards a grand European Commission-backed project known as the Virtual Physiological Human: a computerised replica of the human body that will allow the virtual testing of treatments on patients based on their own specific needs.
Professor Coveney describes this as "the equivalent for the human body of Google Earth". "You could have your own personalised body map … and you could be in charge of managing that and interrogating it yourself," he said.
The creation of an entire virtual human is still many years away. But scientists have already managed to use images of a patient's heart to build virtual arteries, with which they can accurately predict the effectiveness of an operation, such as the insertion of a stent, used to treat heart disease.
"It's not all going to happen overnight, it's going to be incremental. But you should be able to build it up [so] that there are useful components of it along the way," Professor Coveney said of the virtual human project. "As soon as you start digitising, there are applications – it's not just all or nothing."
But there is a problem with computerised medicine: to work properly, it needs patient data, and lots of it. Public trust in this area has been damaged by the troubled history of NHS data projects, the most recent being the botched rollout of the Care.data programme, which has been repeatedly delayed.
Every NHS data scandal that hits the headlines is a major setback for the field of virtual medicine, says Professor Coveney. But he believes that if patients were handed the power to manage their own data, rather than relying on the faceless bosses of their local hospital, they would soon view it as no more sensitive than internet banking.
"You have patients' groups who argue and lobby against data being made available … [but] they are often much more conservative on behalf of the patients than the patients as individuals are," he said. "A lot of patients are very willing to provide their data if you ask them, if there's even a part of a chance that it might help to cure them."
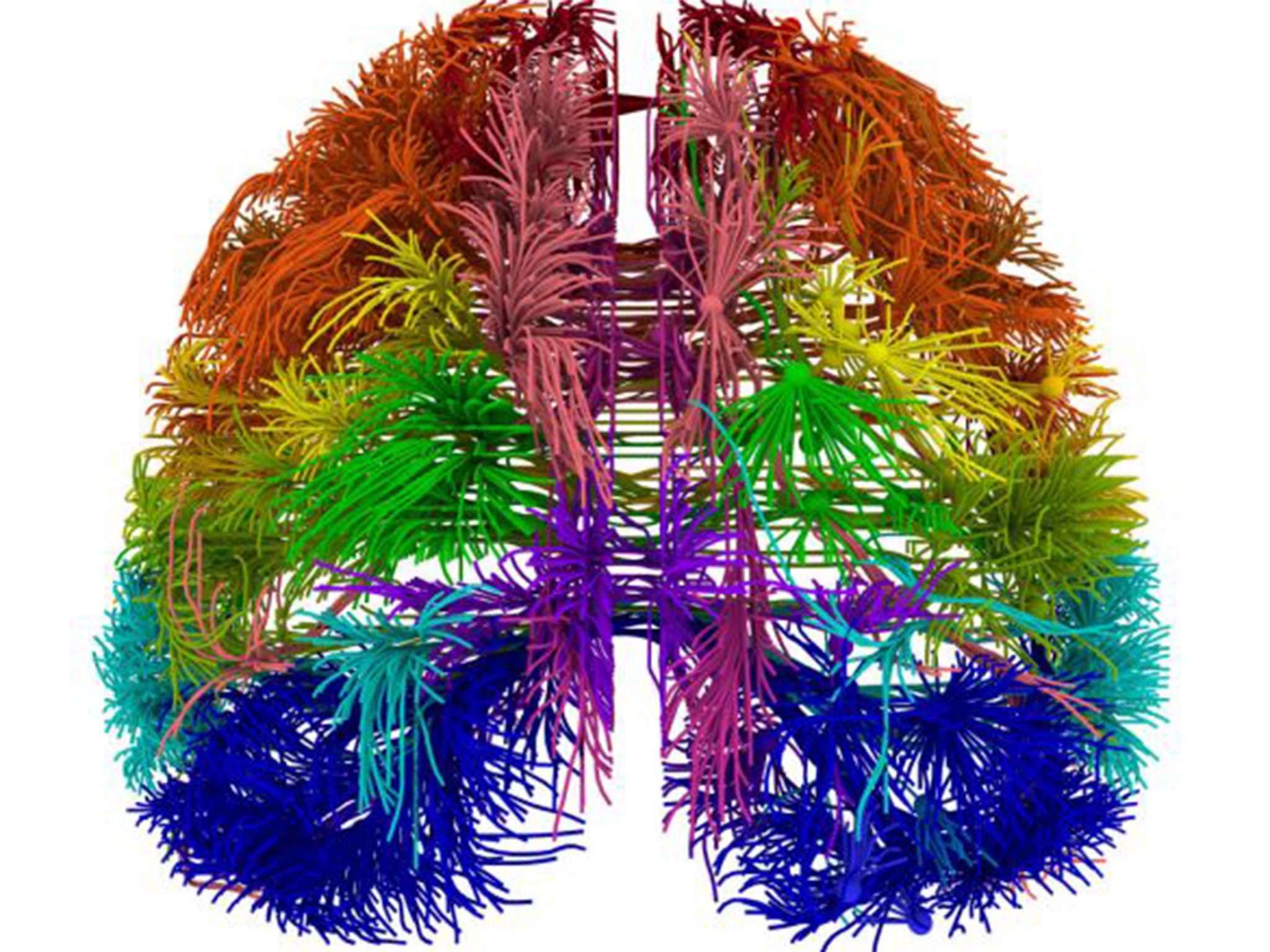
One of Professor Coveney's colleagues is Derek Groen, a postdoctoral researcher whose work concerns modelling the blood flow in a patient's brain. Tapping away on his keyboard at UCL's central London campus, Dr Groen is able to communicate with Archer, the UK's most powerful supercomputer. Based at the University of Edinburgh, it is capable of more than a million billion calculations a second, allowing it to complete the modelling of a patient's blood flow with ease.
The use of supercomputers is vital in this type of work, but not all of them are in the UK. In the future, says Professor Coveney, this could throw up thorny ethical dilemmas. If a computer based in the US makes calculations that result in the death of a patient in the UK, could it be held liable?
Although his PhD was in astrophysics, Dr Groen said he prefers his current work because it could directly benefit people in the short term. "I feel that it's very close to the everyday experience of people and society in general," he said. "I've had people in my family who were affected by strokes – my grandmother, for example, had one at a younger age and another at an older age.
"That's not directly why I'm doing this, but what I do find interesting is... that you get to speak to clinicians and collaborate with them to try and figure things out. For me, that's very motivating."
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies